The US teen birth rate (births per 1,000 females aged 15 to 19 years) has been declining since 1991. Teen birth rates continued to decline from 17.4 per 1,000 females in 2018 to 16.7 per 1,000 females in 2019. This is another record low for US teens and a decrease of 4% from 2018. Birth rates fell 7% for females aged 15 to 17 years and 4% for females aged 18 to 19 years.
Although reasons for the declines are not totally clear, evidence suggests these declines are due to more teens abstaining from sexual activity, and more teens who are sexually active using birth control than in previous years.
Still, the US teen pregnancy rate is substantially higher than in other western industrialized nations, and racial/ethnic and geographic disparities in teen birth rates persist.
Disparities in Teen Birth Rates
Teen birth rates declined from 2018 to 2019 for several racial groups and for Hispanics. Among 15- to 19-year-olds, teen birth rates decreased:
- 5.2% for Hispanic females.
- 5.8% for non-Hispanic White females.
- 1.9% for non-Hispanic Black females.
Rates for non-Hispanic American Indian/Alaska Natives (AI/AN), non-Hispanic Asians, and non-Hispanic Native Hawaiian, and other Pacific Islander teenagers were unchanged.
In 2019, the birth rates for Hispanic teens (25.3) and non-Hispanic Black teens (25.8) were more than two times higher than the rate for non-Hispanic White teens (11.4). The birth rate of American Indian/Alaska Native teens (29.2) was highest among all race/ethnicities.
Birth Rates for Females Aged 15 to 19 Years, by Race and Hispanic Origin of Mother: United States, 2018 and 2019
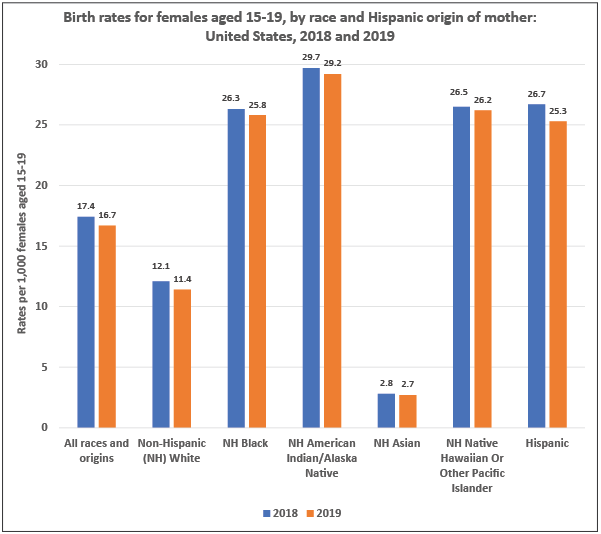
Data source: Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2019. Natl Vital Stat Rep. 2021;70(2):1–50.
Geographic differences in teen birth rates persist, both within and across states. Although among states with low overall teen birth rates, some counties have high teen birth rates.
Social determinants of health, such as low education and low income levels of a teen’s family, may contribute to high teen birth rates. Teens in certain settings are at higher risk of teen pregnancy and birth than other groups. For example, young women living in foster care are more than twice as likely to become pregnant than young women not in foster care.
To improve the life opportunities of adolescents facing significant health disparities and to have the greatest effect on overall US teen birth rates, CDC uses data to inform and direct interventions and resources to areas with the greatest need.
The Importance of Prevention

Teen pregnancy and childbearing are associated with increased social and economic costs through immediate and long-term effects on teen parents and their children.
- Pregnancy and birth are significant contributors to high school dropout rates among girls. Only about 50% of teen mothers receive a high school diploma by 22 years of age, whereas approximately 90% of women who do not give birth during adolescence graduate from high school.
- The children of teenage mothers are more likely to have lower school achievement and to drop out of high school, have more health problems, be incarcerated at some time during adolescence, give birth as a teenager, and face unemployment as a young adult.
- On a positive note, between 1991 and 2015, the teen birth rate dropped 64%, which resulted in $4.4 billion in public savings in 2015 alone.



You must be logged in to post a comment.